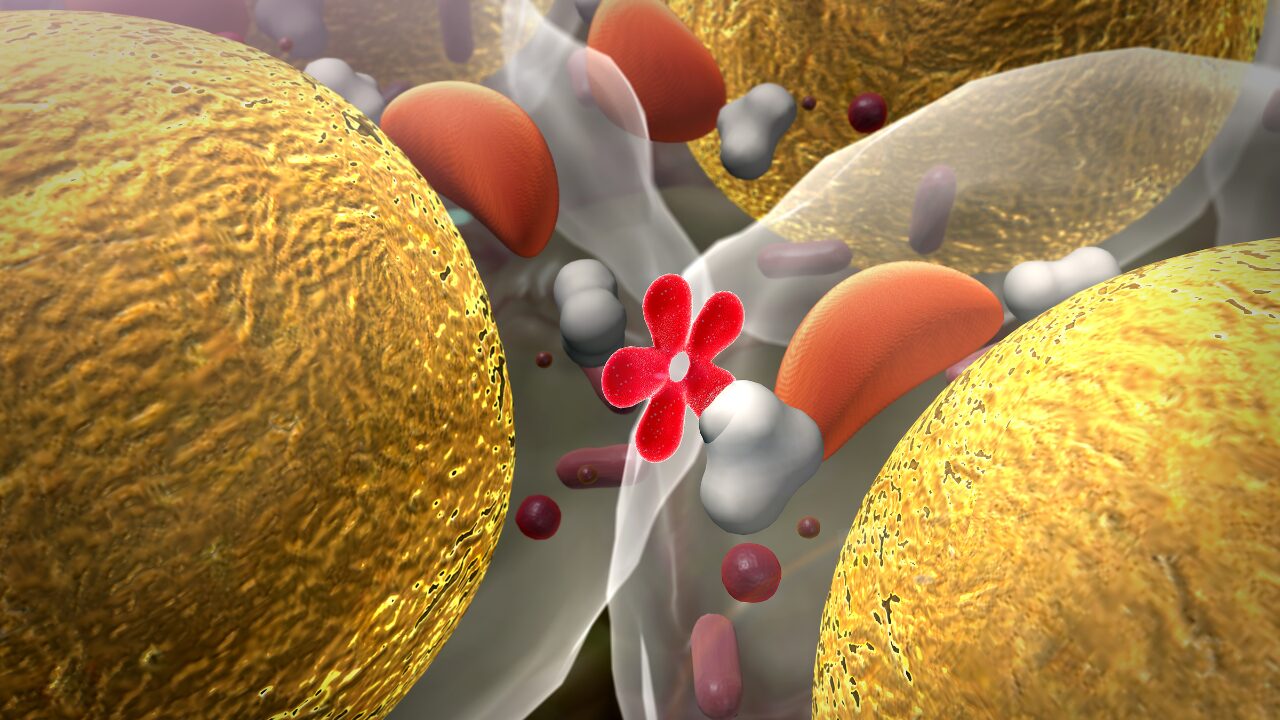
If you’ve been doing all the “right” things—cutting calories, exercising regularly, trying keto or intermittent fasting—but still not seeing results, insulin resistance and inflammation may be overriding your efforts.
When your body is inflamed and insulin-resistant:
-
It’s harder to access stored fat for energy
-
Your metabolism slows down to protect itself
-
Cravings increase due to poor glucose regulation
-
Your stress hormones (like cortisol) rise, further promoting fat storage
-
Detoxification pathways in the liver become sluggish
-
Sleep disturbances prevent recovery and hormone balance
This is why weight loss becomes frustrating and cognitive performance declines, no matter how disciplined your routine.
To reverse this, we need to take a functional medicine approach that focuses on the root causes—not just calories in vs. calories out.